United Health: The Regulatory Reckoning
How UnitedHealth's Optimization Machine Hit the Wall
Regulatory Arbitrage Was the Core Engine:
UnitedHealth's three-decade rise was fueled less by revolutionary care delivery and more by the systematic exploitation of Medicare's risk adjustment coding.
Through vertical integration under Optum, the company built a powerful
infrastructure for reimbursement maximization—an industrial-scale
regulatory optimization machine that outpaced peers in navigating
complex billing systems.
Systemic Shift: Optimization Era Ends:
A confluence of events in 2024–2025—including a DOJ criminal investigation, the CMS’s V28 model overhaul, and a sector-wide earnings shock triggered by Centene
—exposed UnitedHealth’s profit model to be highly dependent on
regulatory complexity. The simplification and tightening of rules turned
the company’s once-formidable scale into a liability, leading to a sharp
valuation decline.
Three Futures, One Reckoning:
UnitedHealth faces three strategic paths: (1) Clampdown Continuation—becoming a low-growth, utility-like healthcare provider; (2) Operational Renaissance—shifting from
billing optimization to genuine care innovation; or (3) Political
Reversal—temporary regulatory relief driven by electoral dynamics.
Each scenario implies a dramatically different valuation and strategic
posture, underscoring the fragility of business models built on regulatory
arbitrage.
I. Prologue: A Promise Made in Minneapolis
(1993)
On a crisp October morning in 1993, Richard Burke stepped to the podium at
the Minneapolis Chamber of Commerce, adjusting his tie as local business
leaders settled into their seats over coffee and Danish pastries. The
UnitedHealth CEO was about to unveil something unprecedented: the first truly nationwide HMO product, spanning all fifty states.
"Ladies and gentlemen," Burke began, his voice carrying the
confidence of a man who believed he was solving one of America's
most intractable problems, "we're not here to manage costs. We're
here to manage care."
The audience applauded politely, but Burke's words carried weight beyond
mere corporate speak. Just months earlier, Warren Buffett had declared
medical costs "the tapeworm of American economic competitiveness" at
Berkshire Hathaway's annual meeting. Here was Burke, promising that
UnitedHealth would be the cure—using private sector efficiency, integrated
networks, and aligned incentives to deliver better outcomes at lower costs.
Thirty-two years later, that promise lies in ruins. UnitedHealth's stock has
collapsed from $594 to $307, the company has withdrawn earnings guidance,
and a Department of Justice investigation looms over its Medicare billing
practices.
The question that haunts Burke's optimistic 1993 vision: Did
UnitedHealth become the solution to America's healthcare cost crisis, or did it
evolve into the most sophisticated parasite the system has ever seen?
II. The Great Optimization (1993-2023)
The three decades following Burke's Minneapolis moment represented one of
the most remarkable value creation stories in American business history.
UnitedHealth grew from a regional HMO to a healthcare colossus with $370
billion in revenues, delivering compound annual earnings growth of 15% while
accumulating a market capitalization that briefly touched $500 billion.
Wall Street celebrated UnitedHealth as the rare company that had "solved"
healthcare—using technology, vertical integration, and data analytics to
extract efficiency from America's $4 trillion medical sector. The Optum
acquisition spree seemed to validate this narrative: primary care physicians,
pharmacy benefit management, data analytics, and payment processing all
brought under one roof, creating what analysts breathlessly described as a
"healthcare operating system."
The company's premium valuation—often trading at 18-20x earnings while
hospital chains languished at 12x—reflected investor confidence that
UnitedHealth had built sustainable competitive advantages. Scale economics,
network effects, and technological sophistication appeared to create an insurmountable moat around the business.
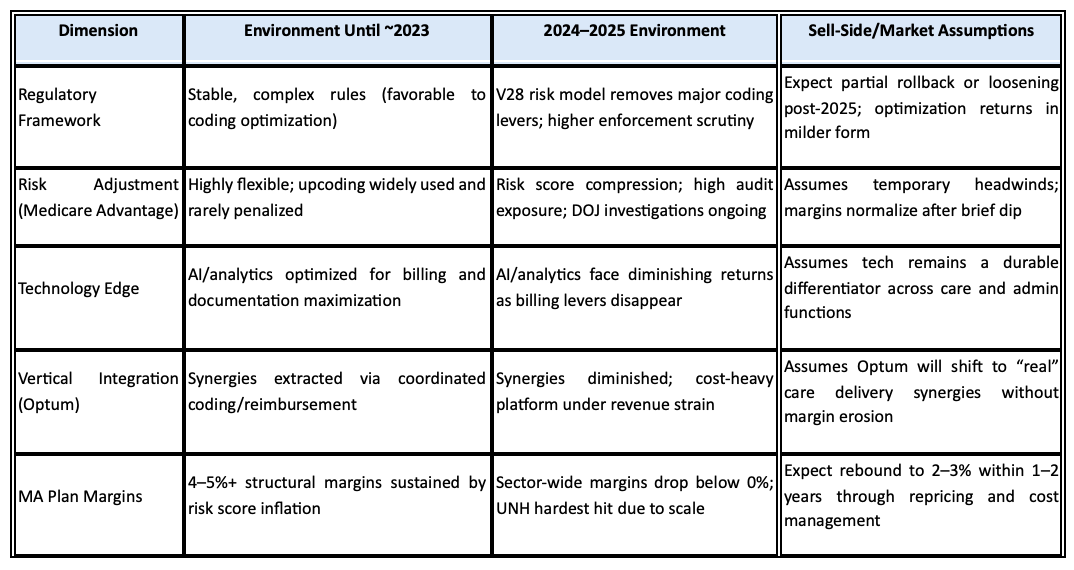
But this narrative, while compelling, obscured the true engine of
UnitedHealth's remarkable performance. The real driver wasn't revolutionary
care delivery or breakthrough cost management. It was something far more
prosaic and, ultimately, far more vulnerable: the systematic optimization of
healthcare's regulatory complexity.
III. The Hidden Engine: Mastering the Machine
To understand how UnitedHealth actually made money, one must delve into
the arcane world of risk adjustment—the mechanism by which the government
pays Medicare Advantage plans more money for sicker patients. Introduced to
prevent cherry-picking of healthy seniors, risk adjustment operates through
diagnostic coding: the more medical conditions a plan documents for its
members, the higher the government payments.
What UnitedHealth discovered, and perfected over two decades, was that
comprehensive documentation could generate revenue increases far beyond
what traditional medical management alone could achieve. Every additional
diagnosis code, properly documented and submitted, translated directly into
higher capitation payments from the Centers for Medicare & Medicaid
Services.
This wasn't fraud—it was optimization. UnitedHealth invested billions in
physician education, coding software, and data analytics to ensure that every
patient interaction captured the maximum allowable diagnostic complexity.
The company's army of nurse practitioners conducting home visits wasn't
primarily focused on improving health outcomes; they were documenting
conditions that supported higher risk scores.
The Optum integration strategy amplified this optimization capability
exponentially. OptumHealth provided primary care physicians who could be
trained in comprehensive diagnostic documentation. OptumRx generated
pharmacy data that revealed undocumented conditions. OptumInsight sold
coding optimization services to other healthcare organizations while
perfecting the techniques for UnitedHealth's own use.
This regulatory arbitrage—converting billing sophistication into consistent
margin expansion—became UnitedHealth's true competitive advantage. While
competitors struggled with medical cost management, UNH focused on
reimbursement maximization within the complex rules governing government
healthcare programs.
The scale effects were profound. Larger organizations could afford more sophisticated coding infrastructure, better training programs, and deeper analytics capabilities. UnitedHealth's size became a regulatory optimization platform, systematically extracting value from Medicare's complexity faster than smaller competitors could match.
IV. Cracks in the Code (2024)
The first hairline fractures appeared in early 2024, though few recognized their
significance at the time. A cyberattack on Change Healthcare, UnitedHealth's payments processing subsidiary, paralyzed medical billing across the United States for weeks. The incident revealed how dependent the entire healthcare system had become on UnitedHealth's infrastructure—and how vulnerable
that infrastructure was to disruption.
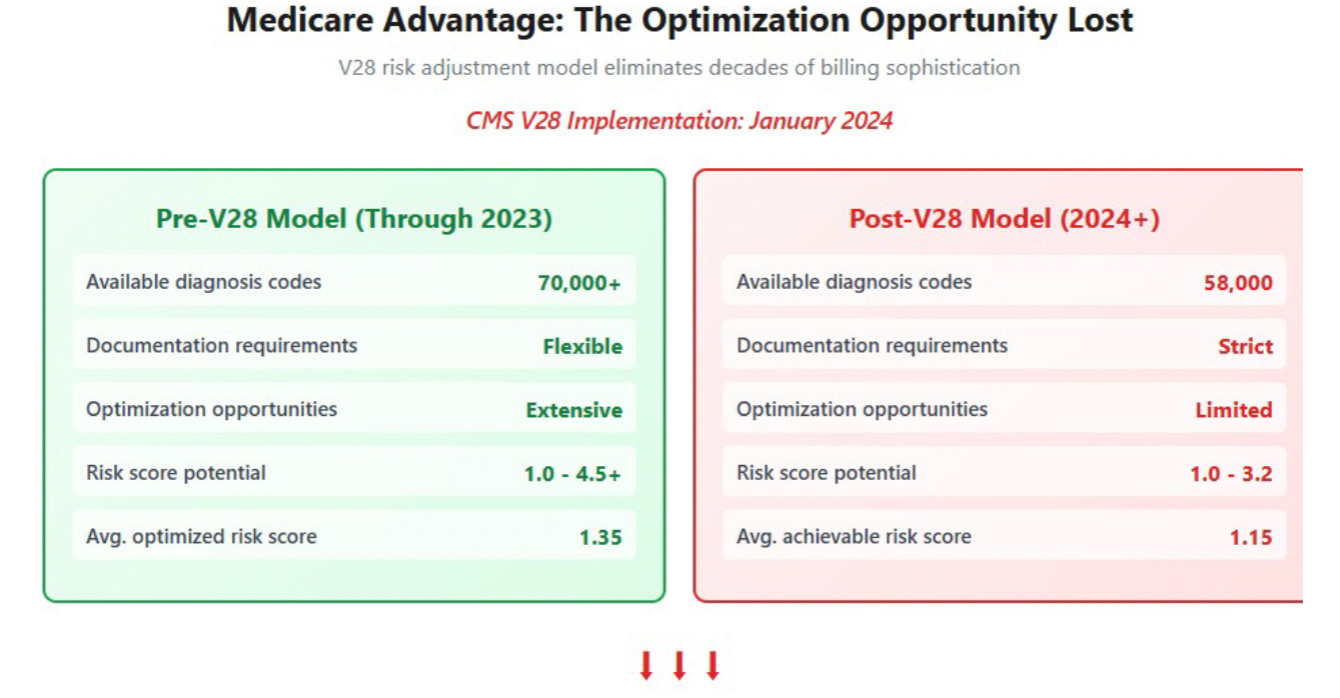
More ominously, the Centers for Medicare & Medicaid Services implemented
the V28 risk adjustment model, quietly eliminating thousands of diagnoses
codes that had been used for optimization purposes. Healthcare policy experts
noted that this change substantially reduced the scope for coding strategies
that had been developed over two decades, but Wall Street largely dismissed it
as a minor administrative adjustment.
Then came the rumors. In March 2025, whispers began circulating about
Department of Justice subpoenas related to UnitedHealth's Medicare
Advantage billing practices. Unlike previous investigations that had resulted in
civil settlements, sources suggested this inquiry was exploring criminal liability
—a fundamental escalation in enforcement philosophy.
UnitedHealth's management dismissed these concerns on quarterly earnings
calls, emphasizing their commitment to compliance and characterizing any scrutiny as routine regulatory oversight. But the company's margins told a different story. Medicare Advantage profitability, which had sustained double-digit returns for years, began showing signs of compression as the optimization playbook faced systematic constraints.
The market, anchored to decades of consistent outperformance, initially interpreted these developments as temporary headwinds. UnitedHealth's stock remained near all-time highs through the first half of 2024, supported by analyst confidence that the company's scale and sophistication would overcome any regulatory challenges.
This complacency would prove catastrophically misplaced.
V. Centene's July 2nd Shock: The Validation
On July 2nd, 2025, Centene Corporation's investor relations team released a
terse press statement that would reverberate across the entire managed care
sector. The company was withdrawing its 2025 earnings guidance and warned
that adjusted earnings per share would fall.
The catalyst wasn't operational missteps or competitive pressure. Recent HHS
program integrity reviews had systematically removed low-utilization, low-cost
ACA enrollees—the exact members who had been subsidizing Centene's risk
pools and enabling profitable growth. In a single policy stroke, years of
optimization-based profit accumulation had been eliminated.
The market reaction was swift and merciless. Centene plunged 40% in pre-
market trading, recording what would become its worst trading day since
2006. But the contagion spread immediately: Molina (-22%), Oscar (-19%), and
UnitedHealth itself (-6%) as investors suddenly grasped that regulatory
tightening affected all government healthcare programs simultaneously.
For UnitedHealth, Centene's crisis provided a devastating validation of the
thesis that optimization-based profits were vulnerable to systematic policy
changes.
If ACA plans could lose 40% of earnings overnight from eligibility reviews, what did that suggest about Medicare Advantage margins facing V28 implementation and potential DOJ enforcement?
VI. When Rules Rewrite Business Models
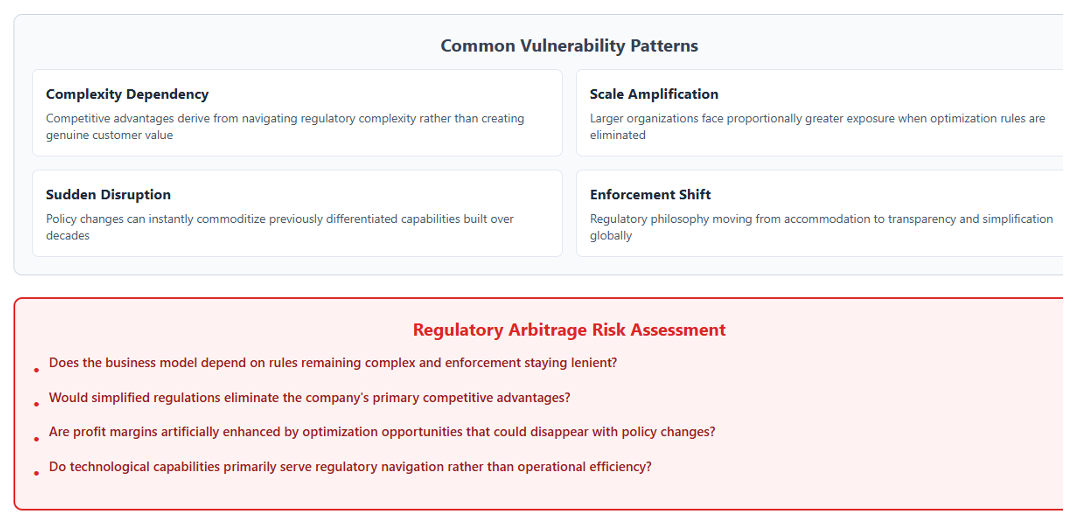
Centene's collapse illuminated a fundamental vulnerability that extends far beyond healthcare: businesses built on regulatory optimization are perpetually vulnerable to rule changes that can eliminate decades of value creation virtually overnight.
This dynamic isn't unique to medical billing.
Consider Europe's General Data Protection Regulation, which destroyed
billions of dollars in adtech value by constraining data collection
practices that had seemed permanently defensible.Or the Basel III banking regulations that forced the dismantling of
proprietary trading operations that had generated consistent profits for
decades
The pattern is consistent: when competitive advantages derive from
navigating regulatory complexity rather than creating genuine customer
value, policy shifts can instantly commoditize previously differentiated
capabilities. UnitedHealth's coding optimization, Centene's ACA risk pool
management, and adtech's surveillance capabilities all shared this
fundamental fragility—they were arbitrage opportunities masquerading as
sustainable business models.
What makes UnitedHealth's situation particularly precarious is the scale at
which this optimization occurred. The company didn't just benefit from
regulatory arbitrage; it industrialized it. Every process, every acquisition,
every technology investment was optimized for extracting maximum value
from Medicare's complexity. When that complexity gets constrained, the entire
integrated platform faces margin compression simultaneously.
The V28 risk adjustment model represents exactly this type of systematic
constraint. By eliminating diagnosis codes and tightening documentation
requirements, CMS has essentially downgraded the regulatory optimization
algorithms that powered two decades of outperformance. UnitedHealth's
sophisticated billing infrastructure, once a competitive advantage, risks
becoming a costly burden in an environment that rewards transparency over
complexity.
VII. Scale as Double-Edged Sword
For thirty years, UnitedHealth's massive scale appeared to provide
unassailable competitive advantages. Larger risk pools enabled better
actuarial predictions. Higher member volumes supported more sophisticated
technology investments. National reach created negotiating leverage with
providers and pharmaceutical companies.
But in the emerging regulatory environment, scale has become a liability
rather than an asset. Consider the contrast between UnitedHealth's national
exposure and regional nonprofit plans like Independence Blue Cross or
Premera Blue Cross. When CMS conducts risk adjustment audits, larger
organizations face proportionally more scrutiny, larger sample sizes, and
higher absolute dollar exposure to clawback.
The political dynamics compound this disadvantage. Regional plans serve
specific communities and maintain relationships with local congressional
delegations. UnitedHealth, as a national for-profit corporation, becomes a
more attractive target for political criticism about healthcare costs and access.
The company's $500 billion market capitalization and executive compensation
packages provide convenient symbols for politicians seeking to demonstrate
action on healthcare affordability.
Moreover, the operational complexity that scale enabled now works against
efficient adaptation. Regional plans can quickly adjust their coding practices,
provider relationships, and benefit designs to comply with new regulations.
UnitedHealth must coordinate changes across thousands of providers, dozens
of markets, and multiple business lines—all while maintaining the integrated
platform that Wall Street values.
This scaling paradox—where size amplifies both opportunity and risk—helps
explain why UnitedHealth's stock has underperformed smaller, regionally
focused plans throughout 2024 and 2025. Investors are beginning to recognize
that in a more transparent, heavily regulated environment, simplicity and focus may triumph over complexity and scale.
VIII. The Three Roads Ahead
UnitedHealth's future trajectory appears to hinge on three distinct scenarios,
each requiring fundamentally different strategic responses and delivering
vastly different investor outcomes.
Clampdown Continuation: This path assumes regulatory tightening
continues across all government healthcare programs, with enforcement
shifting permanently from civil to criminal frameworks. Medicare
Advantage margins stabilize around 2-3% rather than historical 4-6%,
while OptumHealth struggles to generate sustainable profits without
reimbursement optimization advantages. UnitedHealth evolves into a
low-growth utility with stable but unexciting cash flows, trading at 12-
13x earnings like other regulated infrastructure businesses. Stock price
settles in the $300-350 range, reflecting mature industry dynamics and
regulatory constraints.Operational Renaissance: Here, UnitedHealth successfully pivots its
technological capabilities from billing optimization to genuine care
delivery efficiency. The company's data analytics infrastructure enables
meaningful medical cost reductions through better chronic disease
management, preventive care coordination, and provider efficiency
programs. OptumHealth demonstrates authentic value creation
independent of reimbursement optimization, while the integrated
platform delivers the care management synergies that were always
promised but never fully realized. This transformation supports a return
to premium valuations around $400-450, albeit with more modest
growth expectations than the optimization era.Political Reversal: Election-year dynamics and healthcare access
concerns could moderate regulatory enforcement, particularly if
Medicare Advantage enrollment declines significantly. CMS might extend
RADV audit timelines, soften V28 implementation, or provide transition
relief to maintain plan participation. The DOJ investigation concludes
with financial settlements rather than criminal charges, while political
pressure prioritizes healthcare access over billing scrutiny. This scenario
enables partial recovery toward historical business models, supporting
stock prices in the $375-425 range, though with ongoing regulatory
uncertainty.
Each path requires different capabilities and suggests different investment
positioning. The clampdown scenario rewards defensive strategies and
dividend focus. The renaissance path demands patience for multi-year
transformation execution. The reversal case benefits from tactical trading around political and regulatory developments.
IX. Investor Blind Spots: Why Smart Money Missed the Signal
Despite mounting evidence of structural challenges, institutional investors
have been remarkably slow to adjust their UnitedHealth positioning.
Consensus price targets remain anchored near $450—implying confidence that current difficulties represent temporary headwinds rather than permanent
impairment.
Several cognitive biases help explain this persistence in the face of
contradictory evidence. Anchoring effects keep analysts projecting recovery
scenarios based on historical performance metrics that assumed continued
regulatory optimization opportunities. Financial models extrapolating from two
decades of 15% EPS growth struggle to incorporate the possibility that those
growth rates were artificially enhanced by rule arbitrage rather than
operational excellence.
Complexity bias compounds the problem. UnitedHealth's sophisticated
operations, multi-segment integration, and technological capabilities create
an impression of sustainable competitive advantages that are difficult for
competitors to replicate. This sophistication appears durable and defensible,
but much of it was optimized for regulatory navigation rather than care
delivery. When regulations evolve, complexity becomes a burden rather than a
benefit.
Management credibility effects also influence assessment. Stephen Hemsley's
return as CEO has been widely interpreted as stabilizing leadership during a
challenging transition. Hemsley successfully navigated UnitedHealth through
previous regulatory changes and economic cycles, creating confidence that
current challenges are similar to difficulties overcome in the past. However,
systematic regulatory philosophy shifts may require different capabilities than
cyclical operational adjustments.
The investment community's response reflects a broader difficulty in
distinguishing between temporary volatility and permanent disruption.
UnitedHealth's historical track record of overcoming challenges creates strong
priors that current difficulties are surmountable through superior execution.
Acknowledging that competitive advantages were regulatory rather than
operational requires fundamental revision of long-held investment theses.
X. Lessons Beyond Healthcare: The Regulatory Arbitrage Trap
UnitedHealth's predicament offers crucial insights for investors evaluating any
business where profit pools depend on navigating regulatory complexity rather
than creating genuine customer value. The pattern extends across multiple
sectors experiencing similar dynamics.
Financial technology companies that profit from regulatory arbitrage around
banking, payments, or lending regulations face comparable vulnerabilities.
Carbon credit markets, where value derives from interpreting complex rather
than creating genuine customer value. The pattern extends across multiple
sectors experiencing similar dynamics.
Financial technology companies that profit from regulatory arbitrage around
banking, payments, or lending regulations face comparable vulnerabilities.
Carbon credit markets, where value derives from interpreting complex
environmental regulations rather than reducing actual emissions, exhibit similar fragility. Artificial intelligence companies positioning "explainability" and "algorithmic auditing" capabilities as sustainable moats may discover that regulatory clarification commoditizes their differentiation.
The fundamental distinction lies between businesses that create value within
regulatory frameworks versus those that primarily capture value from
regulatory complexity. Companies in the first category tend to maintain
competitive positioning even when rules evolve, because their core value
proposition remains intact. Organizations in the second category face
existential challenges when regulations simplify, clarify, or tighten
enforcement.
UnitedHealth's experience suggests several diagnostic questions for evaluating regulatory arbitrage risk:
Does the business model depend on rules remaining complex and enforcement staying lenient? Would simplified regulations eliminate the company's primary competitive advantages? Are profit margins artificially enhanced by optimization opportunities that could disappear with policy changes? Do technological capabilities primarily serve regulatory navigation rather than operational efficiency?
Businesses answering "yes" to these questions may face similar disruption
when regulatory environments evolve. The optimization era that benefited
UnitedHealth appears to be ending across multiple sectors simultaneously, as
governments worldwide focus on transparency, simplification, and
enforcement rather than complexity and accommodation.
XI. What to Watch Next: The Catalyst Calendar
Several specific developments over the next eighteen months will provide definitive evidence about which scenario is most likely to unfold for UnitedHealth and the broader managed care sector.
September 2025: DOJ charging decisions will signal whether enforcement proceeds along criminal rather than civil paths, fundamentally altering risk assessment for the entire industry.
December 2025: V28 full-year audit results will quantify precisely how
much coding optimization opportunity has been eliminated, providing
concrete measurement of "regulatory alpha" lost.March 2026: 2026 Medicare Advantage bid results will reveal
UnitedHealth's strategic positioning between membership retention andmargin recovery, indicating whether the company can maintain market
share while restoring profitability.June 2026: OptumHealth segment performance will demonstrate
whether provider integration generates sustainable value without
reimbursement optimization advantages, testing the durability of the
vertical integration strategy.Ongoing: CMS rate-setting cycles, RADV clawback invoices, and
congressional oversight hearings will provide continuous signals about
regulatory philosophy and enforcement intensity.
These catalysts will enable real-time assessment of scenario probability rather
than relying on management guidance or analyst projections. The regulatory
environment is evolving faster than corporate adaptation, making external
validation crucial for investment positioning.
XII. Epilogue: Buffett's Tapeworm Revisited
Thirty-two years after Richard Burke's optimistic Minneapolis presentation,
Warren Buffett's healthcare challenge has developed in ways the Oracle of
Omaha likely never anticipated. UnitedHealth did indeed grow to massive
scale and profitability, seemingly validating Burke's promise that private
sector efficiency could solve America's medical cost crisis.
But as we sit in the wreckage of the optimization era—with UnitedHealth's
market cap cut in half, Centene's earnings evaporated, and the entire
managed care sector under regulatory assault—Burke's confident declaration
rings hollow. "We're here to manage care," he had proclaimed, "not
costs."
The uncomfortable truth emerging from the regulatory reckoning is that
UnitedHealth may have done neither. Instead of managing care, the company
optimized billing. Instead of reducing costs, it captured value from complexity.
The sophisticated platform that Wall Street celebrated as healthcare
innovation was, in essence, a regulatory arbitrage machine dressed up as care
coordination.
This doesn't make UnitedHealth villainous—the company operated within legal
frameworks and delivered services that millions of Americans depend upon.
But it does suggest that Burke's 1993 promise was built on a fundamental
misconception about what creates sustainable value in healthcare delivery
The question that haunts UnitedHealth's current crisis extends beyond any
single company to the broader challenge of American healthcare reform:
Can genuine innovation emerge from regulatory constraint, or does the complexity of government healthcare programs inevitably reward optimization over improvement?
Warren Buffett's tapeworm metaphor may have been more prescient than
anyone realized. UnitedHealth didn't eliminate the parasite—it evolved into
the most sophisticated strain the system had ever seen. Whether the
constraint of the optimization era finally creates incentives for authentic
healthcare innovation remains the defining question for American medical
delivery systems.
The Minneapolis Chamber of Commerce luncheon where this story began
represented a moment of tremendous optimism about market-based
healthcare solutions. Today, as regulatory pressure mounts and optimization
strategies face systematic elimination, we're discovering whether that
optimism was justified or whether it simply enabled a more complex form of
the same problem Burke promised to solve.
The answer will determine not just UnitedHealth's future, but the trajectory of
American healthcare delivery for decades to come.
General Legal Disclaimer
This research analysis is based on publicly available documents, company
filings, and third-party media reports through July 3, 2025. Forward-looking
statements and scenario analyses are illustrative projections based on current
information and should not be considered predictions of actual outcomes.
Actual results may differ materially from scenarios described due to regulatory
changes, competitive dynamics, company execution, and other factors
beyond the scope of this analysis. This content is for informational and educational purposes only. Readers should conduct their own due diligence and consult qualified financial professionals before making investment decisions.
All earnings projections, valuation scenarios, and financial calculations are
estimates based on available data and may not reflect actual company performance. Regulatory outcomes, policy changes, and enforcement actions remain uncertain and could significantly impact the scenarios described.